CPT Codes for Remote Therapeutic Monitoring
July 12, 2023
CMS releases its annual Medicare Physician Fee Schedule, which outlines the policies for Medicare reimbursement related to medical practitioner services. In November 2022, CMS announced new policies for Remote Therapeutic Monitoring (RTM) codes that can be furnished under general supervision requirements. This development provides a framework for the implementation of effective RTM services by physicians, nurse practitioners, and physician assistants, utilizing outsourced clinical staff for monitoring and management services. The article will review the RTM codes and Medicare reimbursement for 2023 and best practices for CPT billing code usage in Remote Therapeutic Monitoring.
RTM CODES
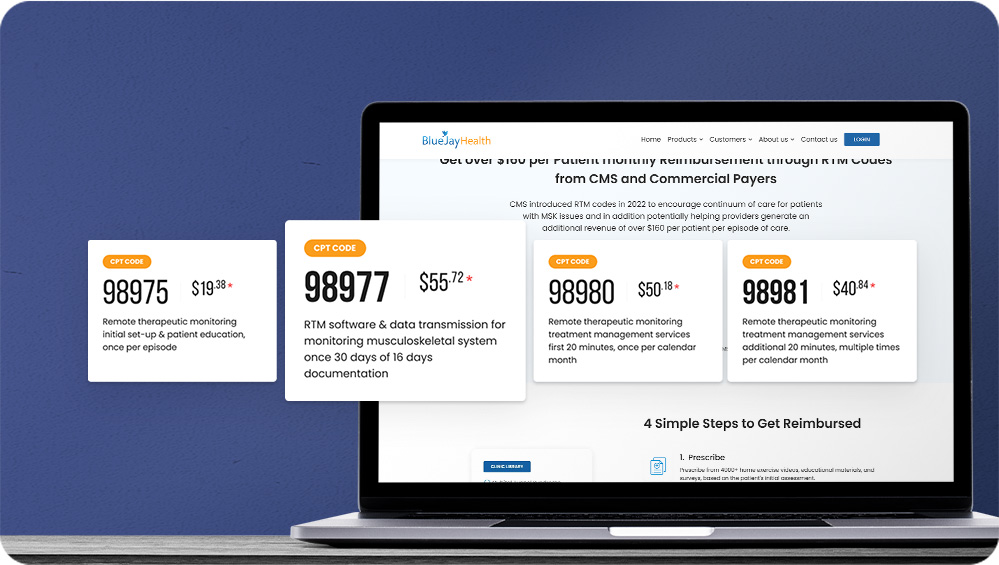
There are 5 CPT codes 98975, 98976, 98977, 98980, and 98981.1
CODE 98975: Initial setup for RTM
This code is used for the initial setup of a monitoring system as well as patient education for using the software. Healthcare providers can claim reimbursement of approximately $19.38 per episode of care under this code. It includes activities such as providing educational material through online platforms. To be eligible for reimbursement, providers are required to continuously track the patient for at least 16 days and receive regular updates on their adherence to the program in each 30 day period.
CODE 98976 / 98977: Track Progress
CPT 98976 and CPT 98977 can be grouped except 98976 is used to monitor patients’ respiratory conditions. CPT 98977 is commonly used by PTs and OTs and allows for reimbursement of up to $55.72 per person per month (30-day period) for musculoskeletal conditions. Data can be collected via medical software as a medical device. Fulfilling the 16-day monitoring requirement within a single 30-day period is advised when submitting claims to the CMS.
CODE 98980/98981: Patient Communication and Multiple RTM Code Submissions
The last two codes on RTM primarily focus on effective communication with the patient. To begin with, providers can utilize CPT 98980 to cover the first initial full 20 minutes of consultation with the patient once a month. Any additional 20-minute consultation that occurs with the patient will be reimbursed under CPT 98981.
For the first 20 minutes of consultation, Medicare offers reimbursement of approximately $50.18. Subsequently, for each additional full 20-minute session with the patient, therapists can expect reimbursement of $40.84 under code 98981.
It's important to note that providers can submit a 98981-code reimbursement multiple times a month for each additional 20-minute session with the patient.
Note:
- Reimbursement amounts listed are a national average based on CMS 2022 non-facility pay rate and are subject to geographic variation.
- Other payers may reimburse for RTM services at different rates. It is important to check with the payer to determine the specific reimbursement amount.
BLUEJAYHEALTH- A QUALITY CARE WITH A TURNKEY RTM REIMBURSEMENT PLATFORM:
BlueJay RTM is a turnkey solution to streamline RTM and support RTM billing.The software solution automates the RTM into 4 simple steps:
- Sending initial setup guides to patients,
- Sending personalized home exercise programs, surveys and educational materials, and automatically tracking patient compliance,
- Facilitating seamless phone calls or telehealth sessions, and
- Managing the reimbursement process.
For more information regarding our RTM solution and its impact on your revenue, Contact us today